Diffuse Axonal Injury (DAI) is a form of traumatic brain injury commonly seen in high speed motor vehicle accidents, assaults (sudden 90-degree rotation of the head), falls, and shaken baby syndrome. In this type of injury, the white matter of the brain (corpus collosum, frontal temporal lobe, and the brainstem) are severely damaged, causing a malfunction in the neurons and their communication with the rest of the brain. Seeking medical attention immediately is highly recommended. The prognosis is poor in patients with severe DAI. Clinical presentation of patients depends on initial assessment of the Glasgow Coma Scale (GCS), which scores patients’ neurological function based on their clinical symptomsandthe severity of DAI. The GCS measures three functions: eye opening (E): 4- spontaneous; 3- response to voice; 2-to pain, and 1-calling the patient’s name. Verbal response (V): 5-normal conversation; 4-oriented conversation, 3-words, but not coherent; 2-no words (only sound); 1- no response. Motor response (M): 6-normal; 5-localized to pain; 4- withdraws to pain; 3- decorticate posture (abnormal posture in which the patient will have his/her arms bent inward towards the body, clenched fist, stiff body, and legs straight).
The initial GCS and the severity of the traumatic brain injury (TBI) help predict the probability of death from the injury. The mortality (death) rate increases the more the GCS score decreases. According to the GCS, a range between 13-15 indicates a mild TBI; a range between 9-12 indicates a moderate TBI ; and a GCS of 8 and below indicates a severe TBI. Mild TBIs may cause concussions and patients may have dementia later in life as a result. Mild to moderate symptoms usually reverse within a few days to weeks after the injury. Sometimes injuries can produce long-term cognitive and behavioral deficits. Consequently, patients who have repeated mild TBIs can have Chronic Traumatic Encephalopathy (CTE). Severe TBIs may have significant risk factors that can be the source of Alzheimer’s disease, Parkinson’s disease, and possibly Amyotrophic Lateral Sclerosis (ALS).
Advanced trauma life support protocol is the standard of care for all head injured patients. (Treatment includes possible resuscitation and neurological treatment performed by a designated neurotrauma center ASAP. Anticoagulation can be used to prevent post-trauma seizures.) The definitive diagnosis is made in post-mortem pathological examination of the brain tissue. In the clinical practice, the diagnosis is made by understanding the cause of the head injury and performingan MRI of the brain. Currently, there are no lab tests to diagnose DAI. Other treatment may involve preventing secondary injuries, such ashypoxia (low oxygen levels caused by difficulty breathing) with hypertension (high blood pressure), swelling, and intracranial hypertension (increased pressure in the brain),that could lead to death, rehab, and supportive care.
DAI can affect both the patient and the patient’s family. The patient may be affected mentally and physically due to the possibility of multiple neurological defects. The quality of life for both the patient and the family may also be affected. The recovery is long. For patients with severe DAI, they will be disabled for the rest of their lives.
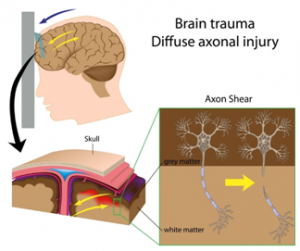
Figure 1: Brain trauma with axon shear.This image depicts damage to the frontal lobe of the brain. In this section of the brain,patients may experience neurological defects in multiple levels of function such as reasoning, planning, problem-solving, long-term memory, social skills, motor function, emotion, judgement, etc.
References
Alila Medical Media. (2019). Brain trauma with axon shear (car accident, shaken baby syndrome.). [Diagram]. Retrieved from https://www.shutterstock.com/image-vector/brain-trauma-axon-shear-car-accident-89651788?src=library
Mesfin FB, Taylor RS. Diffuse Axonal Injury (DAI) [Updated 2019 Nov 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448102/
