In this article, I’m going to talk about frozen shoulder (Adhesive Capsulitis). Shoulder pain can present itself in many ways. You can experience numbness, along with dull, achy, tingling, electrifying sensations that radiates into your shoulders (left, right, or both), and sometimes your scapula. (See these articles for more information: Other Forms of Nerve Pain, Are you experiencing neck pain and Fibromyalgia). You may also have problems lifting or raising your arms above your head. You may be a side sleeper and have shoulder pain every morning. You may have injured your shoulder throwing a ball or trying to prevent yourself from falling.(See other shoulder pain articles for more information: Rotator Cuff Tendonitis, Rotator Cuff Tears, Shoulder Dislocation, Shoulder Impingement, Shoulder Separation, Shoulder Sprain and Strain,SLAP Tear (Superior Labrum Anterior Posterior Tear), Shoulder Fracture, and Shoulder Cartilage Tear). Or, your shoulders may ache before and during a rainstorm, and when there’s colder weather (See articles on Arthritis, Osteoarthritis (OA), and Rheumatoid Arthritis (RA)).
In this article, I will discuss frozen shoulder (Adhesive Capsulitis), which is pain and stiffness in the shoulder that progressively gets worse over time.In the beginning, patients tend to report experiencing pain in the front outer portion of the shoulder and upper biceps region. Patientsmay have limited active (moving your armon your own) or passive (healthcare provider moves your arm for you) range of motion. Eventually the shoulder becomes difficult to move. This process occurs because the connective tissue surrounding the glenohumeral joint (joint capsule) thickens and contracts, causing a decrease in elasticity, and an increase in pain. Patients are afraid to move their arm and shoulder further, thereby causing increased shoulder stiffness and a decrease in synovial fluid that allows the joints to move freely. This first stage tends to last for 6 to 9 months. During the second stage (the Frozen Phase), pain improves but shoulder stiffness may persist for 4 to 6 months. During this stage, patients tend to have difficulty performing activities of daily living such as bathing, washing, combing hair, driving, or carrying heavy objects. During the third stage (the Thawing Phase), patients tend to have improved shoulder mobility. This phase has an estimated 6-months to 2-years recovery period. Frozen shoulder is typically seen in older adults between the ages of 40 and 60 and is seen more in women than men.
Unfortunately, the direct cause of frozen shoulder is unknown. It may occur after injury to the shoulder or inflammation in the soft tissue.(Ex:Bursitis or Tendonitis, Rotator Cuff Tendonitis or Tears), which Frozen shoulder is commonly seen in patients who are immobilized for long periods of time during surgery, and who are recovering from a shoulder fracture. Moreover, frozen shoulder can also be seen in patients with strokes, diabetes, hypothyroidism, Parkinson’s disease, and cardiac disease.
If you suspect yourself or anyone else of having a possible frozen shoulder, follow up with your healthcare provider, for a physical assessment, and shoulder x-ray to assess bone structure and arthritis. A shoulder MRI many be necessary to look at the tissue structure and possible edema (swelling). Treatment for frozen shoulder depends on the outcome of the shoulder assessment and imaging results. If surgery is not required, then continuous physical therapy to maintain mobility and flexibility is the best treatment plan for frozen shoulder. The treatment plan may entaila possible shoulder steroid injection to improve mobility, NSAIDS (Aleve, Advil, Naproxen) to help reduce inflammation and improve mobility, moist heating pads for 20 minutes prior to physical therapy to reduce stiffness, and cold compresses for 20 minutes afterwards to reduce pain and inflammation. However,if non-surgical treatment has not been effective, and the shoulder pain consistently gets worse, follow-up with your healthcare provider for an orthopedic surgical consult.
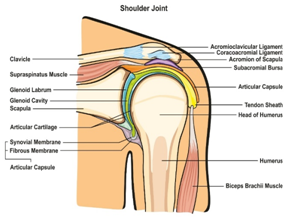
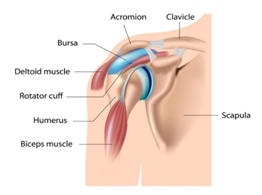
Shoulder Anatomy
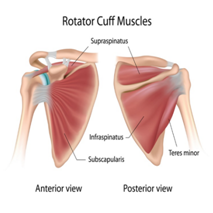
The shoulder is formed where the humerus, collar bone (clavicle), and scapula join. The rotator cuff holds the humerus in place. The muscles that form the shoulder are the supraspinatus, infraspinatus, tres minor, subscapularis, and deltoid. There are four rotator cuff tendons and two biceps tendons that make up the shoulder. These tendons connect the deep layers of the muscles to the scapula and humerus,and provide support to the glenohumeral joint. The supraspinatus tendon is the most affected tendon due to overuse and trauma. The supraspinatus muscle is responsible for lifting the arms out to the side. An injury to this muscle can result in possible rotator cuff tear(s). Overuse can lead to shoulder (subacromial) impingement.
References
Alila Medical Media. (2019). Shoulder bursa, bursitis. [Illustration]. Retrieved from https://www.shutterstock.com/image-illustration/shoulder-bursa-bursitis-122298685?src=LgujqAxYpFEk2V8pW5kcBw-1-8
Alila Medical Media. (2020). Rotator Cuff Anatomy, Labeled. [Illustration]. Retrieved from https://www.shutterstock.com/image-illustration/rotator-cuff-anatomy-labeled-147943874
Prestgaard, T. (2019). Patient education: Frozen shoulder (Beyond the Basics). Retrieved from https://www.uptodate.com/contents/frozen-shoulder-beyond-the-basics
Roberts, J.R. (2018). Adhesive Capsulitis (Frozen Shoulder). Retrieved form https://emedicine.medscape.com/article/1261598-overview
Udaix. (2019). Shoulder Joint of Human Body Anatomy infographic diagram with all parts including bones ligaments muscles bursa cavity capsule cartilage membrane for medical science education and health care. [Drawing]. Retrieved from https://www.shutterstock.com/image-vector/shoulder-joint-human-body-anatomy-infographic-699043855?src=library
