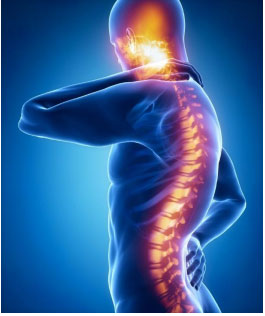
Nerve pain can present in many ways when there is damage or trauma to the spinal cord. In this article, I will identify the other forms of neuropathic pain often seen in the clinical setting and their treatment.
I. Trigeminal Neuralgia
Cause
● Trigeminal neuralgia results from the compression of the fifth cranial nerve (trigeminal nerve).
● It usually occurs on one side of the face but can occur bilaterally.
Signs and Symptoms
● Intense, sharp, stabbing pains can happen without warning.
● Trigeminal neuralgia tends to affect more women than men.
Diagnosis
● An MRI of the brain can indicate this condition.
Treatment
● A neurologist can prescribe treatment.
● First line medication treatments include
o Selective serotonin reuptake inhibitors (SSRIs) for anxiety and depression that are bioproducts of chronic pain.
o Antiepileptics prescribed to prevent seizures from occurring.
o Either carbamazepine or oxcarbazepine to manage the nerve pain.
II. Multiple Sclerosis (MS)
● Multiple sclerosis is a debilitating condition of the brain and the spinal cord.
● The disease occurs in people between ages 20 and 40.
Cause
● MS occurs when the immune system attacks the myelin, a protective sheath that covers the nerve fibers. This attack produces delayed messages between the brain and the rest of the body.
● Over time, the disease will cause permanent damage to the nerves.
Symptoms
Patients with MS experience different symptoms because the severity of the disease is different for each person.
● A decline in the ability to walk
● Visual disturbances
● Muscle weakness
● Numbness
● Tingling
● Memory loss
● Lost ability to write and speak
Treatment
● Currently, there is no standardized test or cure for multiple sclerosis.
● It is important that patients continue to be as active as possible.
● Physical therapy and occupational therapy are beneficial.
III. Traumatic Spinal Cord Injury (Incomplete Spinal Cord Injury)
Traumatic spinal cord injury is damage to any part of the spinal canal or nerves.
Causes
● An acute trauma (e.g., a fall or injury from a motor vehicle accident)
● Injury from lifting heavy objects improperly
● Contact sports
Symptoms
● Temporary or permanent loss of strength
● Decline in extremity mobility
● Increased neuropathic and radicular pain that radiates down the extremities and spine
Diagnosis
● MRI or CT scan of the injured spinal area Treatment
● Treatment depends on the severity of the damage to vertebral, tissue, and ligaments as indicated by results of the MRI or CT scan of the injured spinal area.
● Constant follow up with your primary care physician, general practitioner, pain management specialist, and neurosurgeon are important.
IV. Radiculopathy (Pinched Nerves)
Radiculopathy is a condition that accompanies all spinal cord injuries. It occurs when one or more of the affected nerves do not work properly.
Causes
● Narrowing of the foramina (space where the nerves exit the spinal column and innervate the muscles)
● Spinal stenosis
● Bone spurs
● Herniated discs
Symptoms
● Chronic radicular pain results in muscle weakness
● Difficulty controlling extremities
● Numbness
Treatment
● Find the underlying cause by following up with your primary care physician or general practitioner who can order X-rays and an MRI or CT.
● Gabapentin or Lyrica will be helpful in managing neuropathic pain.
● If pain is intolerable, a referral to a pain management specialist is necessary for epidural steroid injections (ESIs).
● If there is severe nerve impingement or compression present, and the patient has a severe decline in neuromuscular function, a neurosurgeon consultation is necessary.
V. Complex Regional Pain Syndrome (CRPS)
Symptoms
Characteristics of CRPS
● CRPS consists of multiple pain symptoms that include allodynia (sensitivity to touch) and hyperalgesia (increased sensitivity to pain).
● CRPS can also cause loss of function.
● CRPS is rare, is seen mostly in the lower extremities, and occurs in more females than males.
Treatment
● The goal of the treatment plan for complex regional pain syndrome is to continue to have improved function.
● Physical therapy, along with the management of depression and anxiety that may accompany the condition, must be a part of the treatment plan.
● Use of Gabapentin, Lyrica, or Amitriptyline for managing neuropathic pain may also be necessary.
VI. Phantom Pain and Amputation
● People who have had an extremity amputated (hands, arms, fingers, toes, breasts, legs) will experience phantom pain.
● Phantom pain is not a mental health issue; however, chronic pain can affect amputees mentally, physically, and socially.
● Phantom pain is a sensation that amputees feel after having a body part removed.
Cause
● Researchers believe that the underlying cause of phantom pain is the regeneration of new nerves in response to the nerves that were severed during the amputation.
Symptoms
● New amputees will experience this pain (sharp, stabbing, dull, throbbing, or burning) a few hours after the amputation.
● The pain may be continuous or intermittent and felt distally to the missing extremity.
Treatment
● Support groups
● Physical therapy
● Pain management
● Counseling
● Education
References
American Chronic Pain Association. (n.d). Neuropathic Pain. https://www.theacpa.org/conditions-treatments/conditions-a-z/neuropathic-pain/
Cliparea. (2019). Spine injury pain in sacral and cervical region concept. [Illustration]. https://www.shutterstock.com/image-illustration/spine-injury-pain-sacral-cervical-region-375666790?src=cBY_eytOMl-FKiy1I1NONA-3-33
