Iliotibial Band Syndrome (ITBS). Do you love to run? Have you ever had a burning, achy, tenderness on the outside of your knee after running? Do your knees get stiff and swell? Do you have pain in your hips or on the lateral portion of your thighs? If you answered yes to any of these questions, then you may have iliotibial band syndrome (IBTS). I have had IBTS a few times and the treatment process is not fun. Sometimes, the pain can flip-flop from one side to the thigh to the other. Through my recovery process, I learned that daily stretching is key to preventing its return. To learn more about ITBS, read the detailed information below.
What is iliotibial band syndrome (ITBS)?
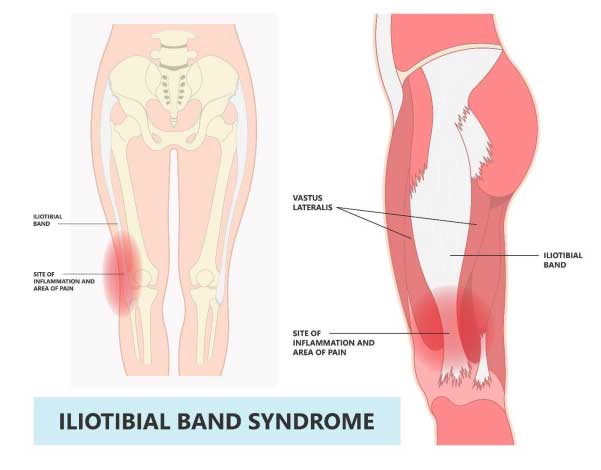
● Iliotibial band syndrome is the most common cause of lateral knee pain among athletes.
● The cause of ITBS is inflammation of the bursa surrounding the iliotibial band (ITB).
● This injury affects athletes whose sports require continuous running or repetitive knee flexion and extension.
o Examples of sports include long-distance running, cycling, volleyball, tennis, soccer, football, skiing, weightlifting, and aerobics.
Signs and symptoms
● Pain on the lateral (outer) knee is present with running.
● Early onset of pain resolves after running.
o If athletes continue to run during the early onset of the injury, then the pain will progressively be present during walking and training sessions.
● Pain is located over the lateral femoral epicondyle.
● Untreated pain may radiate to the distal tibia, calf, and up to lateral thighs.
● Pain is present while walking upstairs or running downhill.
Causes
For runners:
● The posterior (back) edge of ITB impinges against the lateral epicondyle of the femur just after the foot strikes the gait cycle.
● The injury usually occurs after 30 degrees of knee flexion (bend).
● Downhill running and jogging slowly may exacerbate ITBS because the knee tends to be less flexed at the foot strike.
● Other causes include the following:
o Running on hard surfaces and banked surfaces
o worn out or improper running shoes
o foot misalignment
o leg-length discrepancy.
For cyclists:
● The ITB has pulled anteriorly (front) on the pedal downstroke and posteriorly on the upstroke.
● The ITB is predisposed to friction, irritation, and microtrauma during repetitive movements because posterior fibers adhere closely to the lateral femoral epicondyle.
● A cyclist with external tibia rotation greater than 20 degrees puts stress on the ITB if the cycling shoe is pointed in a straight position or the toe is in a cleat position.
● Vargus knee alignment occurs when the cyclist actively pronates and places a greater stretch on the distal ITB when using internally rotated cleats.
● A poorly fitted bicycle saddle that extends the knees greater than 150 degrees causes the knee to extend the distal ITB to rub across the lateral femoral condyle.
For all athletes:
● Improper warm-up and stretching
● Increasing the quality and quantity of training sessions too quickly
● Leg length discrepancy
● Worn out or improper athletic shoes
Treatment
● Consult with a primary care provider, sports medicine specialist, or orthopedic specialist if you suspect this injury.
● Begin physical therapy to decrease inflammation and implement a stretching program.
● Focus on controlling inflammation.
● Correct poor training habits.
● Use NSAIDs (ibuprofen (Advil) or naproxen (Aleve)) to help manage the pain.
● Reduce stress on the knee.
● Avoid participating in activities that caused the injury.
● Consider surgery when prolonged conservative treatments have failed to alleviate the symptoms or resolve ITBS.
Recovery
● Athletes can return to play when pain has resolved, they have achieved normal flexibility of ITB, and they have regained full strength of hip and knee muscles.
Complication
● If athletes do not make a full recovery, then ITBS can be a chronic condition.
Prognosis
● The prognosis for athletes is excellent if they maintain ITB flexibility and correct factors that can cause this injury.
References
Cleveland Clinic. (2022). Iliotibial Band Syndrome. https://my.clevelandclinic.org/health/diseases/21967-iliotibial-band-syndrome
Pepermpron. (2022). [Illustration]. Stretching treat athlete tear sprain muscle inflammatory runner cycling hiking shot knee hip pain sport IT band Pes bursa tract medial soccer tibia femoris RICE Rest ice elevation method strain. https://www.shutterstock.com/image-vector/stretching-treat-athlete-tear-sprain-muscle-2139432651
Stirling, Jerold M. (2018). Iliotibial Band Syndrome. https://emedicine.medscape.com/article/91129-overview
